Debunking Pain Management Myths
Pain management, a vital component of healthcare, is often misunderstood due to prevalent myths and misconceptions. These myths range from beliefs about the nature and severity of pain to the effectiveness of various treatments.
Addressing these misconceptions is essential for improving pain management strategies and patient outcomes. This article aims in debunking pain management myths, from the overuse of opioids to the belief that pain is an inevitable part of aging.
By clarifying these misconceptions, we hope to promote a more informed, effective, and patient-centered approach to pain management.
Table of Contents
Myth 1: Pain is All in the Mind
Reality: Pain is a complex experience involving physical, psychological, and sometimes social factors.
It often has a physical basis, such as injury or inflammation, and is the result of signals sent from the body to the brain. While psychological factors like stress and mood can influence how pain is perceived and managed, they do not negate its physical reality.
The brain's role in interpreting pain signals does not mean the pain is imaginary. Chronic pain conditions illustrate the complexity of the relationship between physical and psychological factors, often involving changes in the nervous system that persist beyond the initial injury.
Understanding that pain is not just "all in the mind" is crucial for effective pain management, leading to more comprehensive and empathetic treatment approaches that address the multifaceted nature of pain.
Myth 2: Stronger Pain Equals More Severe Health Issues
Reality: Pain perception varies greatly among individuals and is influenced by factors such as personal pain tolerance, emotional state, and past pain experiences.
For example, conditions like fibromyalgia or migraines can cause intense pain without signaling a life-threatening situation. On the other hand, serious illnesses such as certain cancers may not cause significant pain in their early stages. The intensity of pain is not a reliable measure of the severity of a medical condition.
Psychosomatic pain, which arises from emotional and psychological factors, further complicates this relationship, as it can be severe but not indicative of a physical ailment in the traditional sense. These insights highlight the importance of a comprehensive medical assessment that goes beyond pain intensity to accurately diagnose and treat the underlying cause of pain.
Understanding this disconnection between pain intensity and health severity is crucial for providing accurate diagnoses and effective treatment plans tailored to individual patient experiences.
Myth 3: Opioids are the Best Solution for All Types of Pain
Reality: While opioids can be effective for certain types of pain, particularly acute and cancer-related pain, they are not suitable for all pain conditions due to their high risk of dependence, addiction, and other side effects.

This is particularly true for chronic non-cancer pain. Different types of pain, like neuropathic or inflammatory pain, may respond better to other treatments such, as non-opioid medications, physical therapy, or interventions targeting nerve function.
Effective pain management often requires a multimodal approach, which may include a combination of medication, physical therapy, psychological support, and lifestyle changes.
Personalizing treatment plans to the individual's specific needs and conditions is essential for effective pain management. This understanding shifts the focus from a reliance on opioids to a more comprehensive, safer, and individualized approach to pain management.
Myth 4: Over-the-Counter Painkillers are Completely Safe
Reality: While generally safe when used as directed, these medications can have risks and side effects, especially with misuse or prolonged use.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin can cause gastrointestinal issues and kidney damage and increase the risk of heart problems. Acetaminophen (Tylenol) can lead to liver damage if taken in high doses or combined with alcohol.
There's also the risk of overuse or misuse, particularly for chronic pain, where people might exceed the recommended dosage or duration of use without medical advice. OTC painkillers can interact with other medications, potentially leading to adverse effects. Moreover, they may not be effective for all types of pain, such as certain chronic or neuropathic pains.
Understanding these risks encourages responsible use of OTC painkillers and consultation with healthcare professionals for persistent, severe, or specific pain types. This awareness is crucial for safer use and better pain management practices.
Myth 5: Rest is the Best Cure for Pain
Reality: While rest is important, especially following an injury or during acute pain phases, it is not always the most effective strategy for managing pain in the long term.
Prolonged rest can lead to muscle weakness, stiffness, and overall deconditioning, which might worsen some types of pain, especially chronic musculoskeletal pain. It can also negatively affect mental health. Active pain management strategies, such as physical therapy and gentle exercise, are often more beneficial.
These activities help maintain or improve muscle strength and flexibility and promote blood circulation, aiding in recovery. The key is to strike a balance between rest and activity, as both overexertion and prolonged inactivity can exacerbate pain.
The best approach varies depending on the type and cause of pain, as well as the individual's overall health and fitness level. Healthcare providers should tailor their recommendations to each patient's specific condition and capabilities.
Dispelling this myth promotes a more effective, balanced, and individualized approach to pain management, emphasizing the importance of a dynamic treatment strategy that includes appropriate rest and physical activity.
Myth 6: Pain is Inevitable with Aging
Reality: While older adults may experience more frequent aches and pains due to conditions like arthritis, osteoporosis, and musculoskeletal disorders, severe or chronic pain is not a normal aspect of aging.
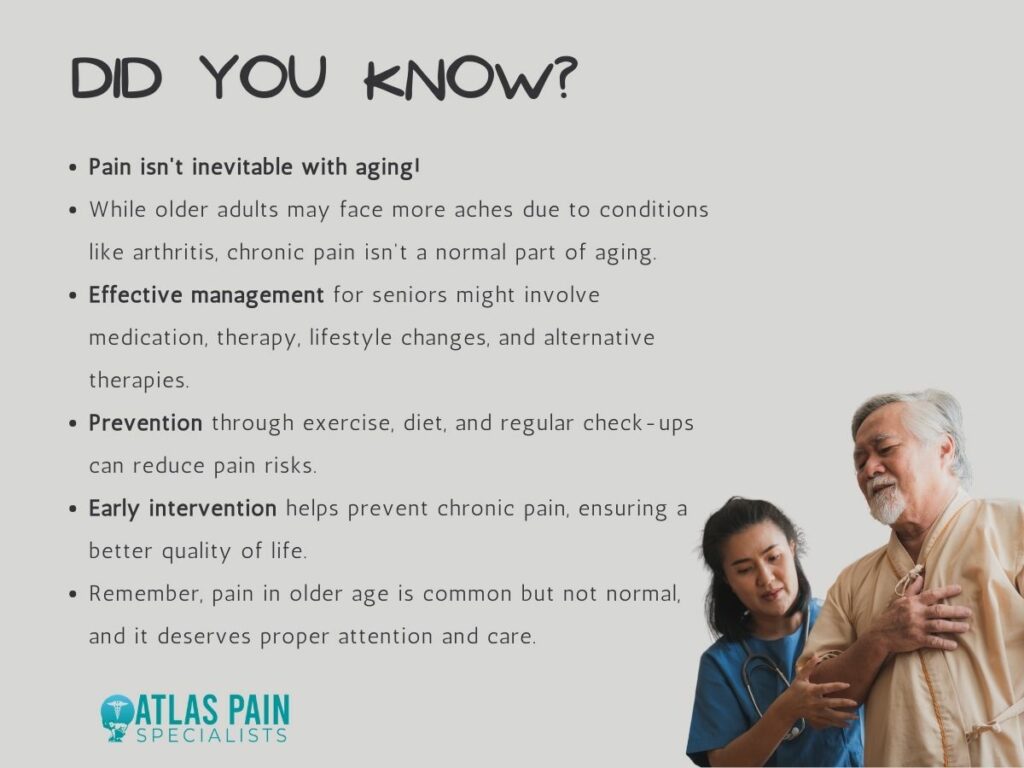
Treating pain as inevitable can lead to its under-treatment or mismanagement in older adults, negatively impacting their quality of life. Effective pain management for the elderly might require a different approach than for younger individuals, often involving a combination of medication, physical therapy, lifestyle changes, and possibly alternative therapies.
Preventive measures such as regular exercise, a healthy diet, and regular medical check-ups are important in reducing the risk of conditions that cause pain. Early intervention is also crucial in preventing pain from becoming chronic.
Dispelling this myth emphasizes the importance of proactive, tailored pain management strategies for older adults, improving their overall quality of life and underscoring that, while pain may be more common in older age, it is not an acceptable or normal part of aging.
Myth 7: Chronic Pain is Always Visible
Reality: Many chronic pain conditions are 'invisible,' meaning they do not manifest in outward, visible signs.
Conditions like fibromyalgia, migraine, neuropathic pain, and certain autoimmune diseases can cause significant discomfort and disability without visible symptoms. This invisibility often leads to misunderstanding, stigma, and the underestimation of the severity of the pain, causing psychological distress and isolation for those suffering.
Recognizing and validating the experiences of individuals with chronic pain is crucial, even in the absence of visible signs. Effective management of chronic pain requires a comprehensive approach that includes medication, physical therapy, psychological support, and lifestyle changes, addressing both the physical and psychological aspects of the condition.
Dispelling this myth is essential for a more empathetic and effective approach to pain management, emphasizing the need for holistic treatment and support for those experiencing chronic pain.
Myth 8: Ignoring Pain Will Make it Go Away
Reality: Pain is a signal from the body indicating an underlying issue, and neglecting it can exacerbate the condition, potentially leading to more severe consequences.
Untreated pain, especially if chronic or severe, can evolve into chronic pain syndromes, making the body more sensitive to pain stimuli and harder to treat over time. Early intervention is crucial, as timely and appropriate treatment can address the root cause of pain and prevent it from becoming a long-term problem.
Ignoring pain also has a significant psychological impact, potentially leading to anxiety, depression, and a reduced quality of life. It can affect daily activities and social participation. Effective pain management often requires a combination of approaches, including medication, physical therapy, and psychological counseling.
Recognizing the need to address pain promptly and comprehensively is essential for preventing the development of chronic conditions and achieving better overall outcomes and quality of life.
Myth 9: Pain Medication is the Only Treatment
Reality: Effective pain management often requires a multifaceted approach that goes beyond just medications.

Non-pharmacological treatments such as physical therapy, acupuncture, massage therapy, and mind-body techniques like meditation and relaxation exercises can be highly effective in managing pain. Lifestyle modifications, including regular exercise, a healthy diet, and adequate sleep, are also crucial in pain management.
Psychological support, such as cognitive-behavioral therapy (CBT), plays a significant role, especially in chronic pain, by helping patients develop coping strategies and change negative thought patterns related to their pain.
A multidisciplinary approach that combines different therapies and treatments, tailored to the individual's specific needs and pain type, is often the most effective.
Dispelling this myth is important for a more comprehensive understanding of pain management, emphasizing the need for holistic strategies that encompass both pharmacological and non-pharmacological methods, lifestyle changes, and psychological support.
Myth 10: You Just Have to Live With Chronic Pain
Reality: Advances in pain management have shown that chronic pain, while not always curable, can often be managed effectively.
Management strategies include medication, physical therapy, psychological counseling, lifestyle modifications, and in some cases, surgical interventions or advanced therapies like nerve blocks or spinal cord stimulation. Ongoing research and technological advancements continue to improve the understanding and treatment of chronic pain.
A patient-centered approach, considering the individual's unique pain experience, lifestyle, and overall health, is essential. This often involves a combination of treatments and adjustments based on the patient's response. Educating patients about chronic pain and involving them in their treatment plans is crucial for empowerment and effective management.
Dispelling this myth is important for encouraging proactive and effective pain management, highlighting the need for comprehensive, adaptive, and patient-focused strategies in managing chronic pain.
Conclusion
Debunking these common pain management myths is essential for advancing a more effective and compassionate approach to treating pain.
By understanding that pain is a complex and individual experience, not merely a symptom to be silenced, we can adopt more holistic and tailored treatment strategies. This includes recognizing the limitations and risks of opioids, the potential of non-pharmacological interventions, and the importance of addressing both physical and psychological aspects of pain.
Ultimately, dispelling these myths fosters a more informed, patient-centered approach to pain management, contributing to better health outcomes and improved quality of life for those suffering from pain.
About Dr. Sean Ormond