Pain Management for Diabetic Neuropathy
Diabetes-related neuropathy is one of the many issues that can emerge from having diabetes. Diabetic neuropathy is a form of peripheral nerve degeneration that affects people with diabetes and causes a variety of symptoms. Pain Management for Diabetic Neuropathy is crucial.
Among these symptoms, one of the most pervasive and debilitating is neuropathic pain. Understanding the complexities of diabetic neuropathy and implementing effective pain management strategies are crucial components of enhancing the quality of life for those affected.
According to recent statistics, a significant percentage of individuals with diabetes experience some form of neuropathy during their lifetime. Given the complication's broad prevalence, thorough pain management measures are needed in order to reduce suffering and enhance overall quality of life.
Understanding Diabetic Neuropathy
Diabetic neuropathy is a long-term complication of diabetes that arises due to prolonged exposure to high levels of blood sugar. It affects various nerves throughout the body, with the peripheral nerves commonly being involved.
Diabetic neuropathy is a complex and multifaceted complication that arises from prolonged exposure to elevated levels of blood sugar, a hallmark of diabetes. This condition affects the peripheral nerves, which are crucial in transmitting signals between the central nervous system and the rest of the body.
The impact of diabetic neuropathy extends beyond mere discomfort, often leading to significant impairments in sensory, motor, and autonomic functions. The prevalence of diabetic neuropathy underscores the significance of addressing its impact on individuals living with diabetes.
- Causes and risk factors
The primary cause of diabetic neuropathy is prolonged hyperglycemia, where high levels of glucose in the blood lead to damage to the nerve fibers. However, the development and severity of neuropathy can be influenced by various factors.
These include the duration of diabetes, inadequate blood sugar control, genetics, and lifestyle factors such as smoking and excessive alcohol consumption.
- Common symptoms
Diabetic neuropathy manifests in a variety of symptoms, and the specific presentation can vary among individuals. Peripheral neuropathy, the most prevalent form, often results in sensations of pain, tingling, and numbness, usually starting in the extremities.
Autonomic neuropathy can affect involuntary bodily functions, leading to issues like digestive problems, blood pressure fluctuations, and sexual dysfunction. Motor neuropathy may cause muscle weakness and difficulty in coordination.
Pain Management Strategies
Diabetic neuropathy pain must be effectively managed using a multimodal strategy that takes into account both the underlying causes and symptoms of the condition. Various strategies, ranging from pharmaceutical interventions to lifestyle modifications, play a crucial role in providing relief and improving the quality of life for individuals grappling with neuropathic pain.
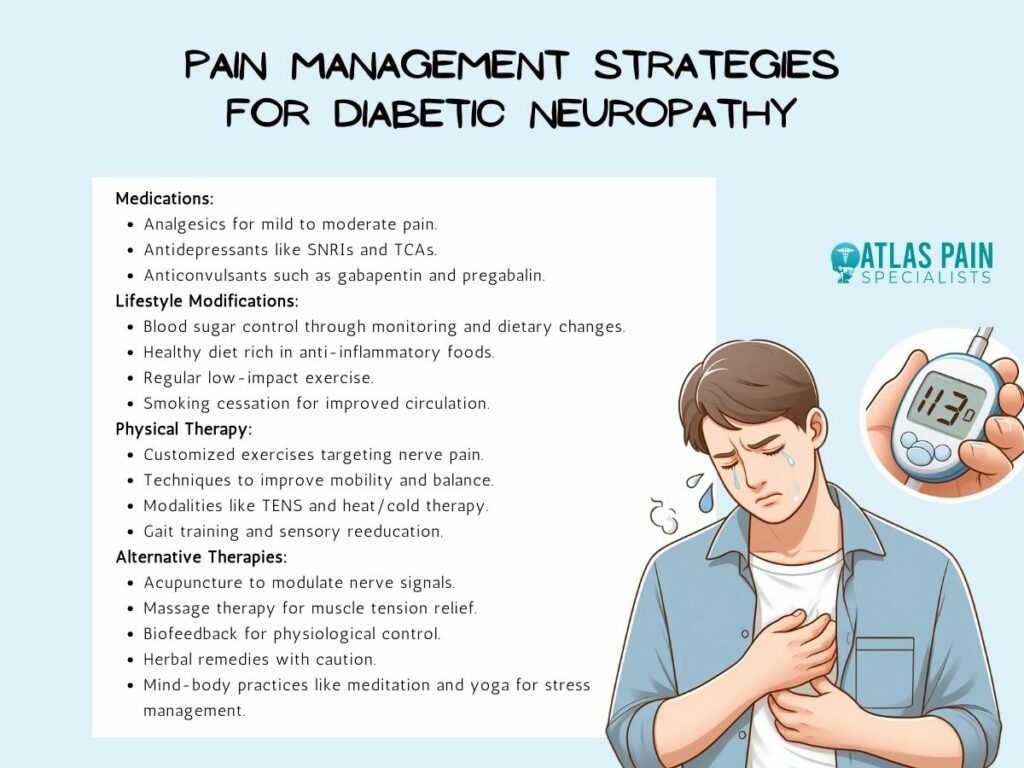
- Medications for Diabetic Neuropathy
The pharmacological approach aims to modulate the transmission of pain signals, alleviate symptoms, and improve overall quality of life. Several classes of medications have shown efficacy in addressing the complex nature of neuropathic pain.
While these medications provide relief, their efficacy can vary among individuals, and a personalized approach to medication selection is crucial. The choice of medication depends on factors such as the nature and severity of symptoms, individual tolerance, and the presence of other medical conditions.
- Analgesics
Analgesic medications, including acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), are often employed for mild to moderate neuropathic pain relief. While these medications can be effective, it's essential to consider their limitations and potential side effects.
Long-term use of NSAIDs, for instance, may pose risks to the gastrointestinal system and renal function.
- Antidepressants
Neuropathic pain can be effectively treated with selective serotonin and norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs). Amitriptyline, a TCA, and duloxetine, an SNRI, are commonly prescribed.
These medications alter neurotransmitter levels in the brain, influencing the perception of pain signals. However, side effects such as dry mouth, dizziness, and sedation should be monitored.
- Anticonvulsants
Medications traditionally used to control seizures, such as gabapentin and pregabalin, have emerged as valuable options for neuropathic pain management. These anticonvulsants stabilize nerve cell membranes, modulating abnormal signaling that contributes to pain.
Careful titration is necessary to manage side effects like dizziness and drowsiness.
- Lifestyle Modifications
These modifications aim to address underlying factors contributing to nerve damage, enhance overall health, and optimize the effectiveness of pain management strategies. Implementing these lifestyle modifications requires a proactive and collaborative effort between individuals with diabetes, healthcare providers, and support networks.
Tailored care plans that take into account the distinct requirements and inclinations of every person can improve compliance with these lifestyle adjustments.
- Blood sugar control
The key to avoiding and treating diabetic neuropathy is achieving and sustaining appropriate blood sugar levels. For general health and well-being, it is necessary to regularly check blood glucose levels, take prescribed medications as directed, and make lifestyle changes, including eating a balanced diet.
- Healthy diet and nutrition
Making healthy dietary decisions is essential for controlling diabetic neuropathy. An anti-inflammatory and vitamin- and mineral-rich diet promotes the health of your nerves.
Foods rich in omega-3 fatty acids, such as walnuts, flaxseeds, and fatty fish, have anti-inflammatory qualities that may help those with neuropathic pain.
- Regular exercise
Engaging in physical activity is important for managing diabetes and is crucial in reducing neuropathic pain. Frequent exercise lowers inflammation, increases blood circulation, and aids in blood sugar regulation.
For those with neuropathy, low-impact activities like swimming, cycling, or walking are ideal since they improve general fitness without putting undue strain on the joints.
- Smoking cessation
Smoking is a huge risk factor for the development and progression of diabetic neuropathy.
Quitting smoking is a crucial lifestyle modification that not only benefits neuropathic pain management but also contributes to overall cardiovascular health, minimizing the risk of additional complications. The harmful components of tobacco can exacerbate nerve damage and hinder circulation.
Quitting smoking is a crucial lifestyle modification that not only benefits neuropathic pain management but also contributes to overall cardiovascular health, minimizing the risk of additional complications.
- Physical Therapy
Physical therapy is a key component of pain management for diabetic neuropathy, offering targeted interventions to improve mobility, alleviate discomfort, and enhance overall quality of life. Physical therapy sessions are typically tailored to the individual's specific needs, taking into account the severity of neuropathic symptoms, overall health, and personal goals.
The collaborative nature of physical therapy empowers individuals to actively participate in their pain management, providing them with tools and knowledge to continue exercises independently at home.
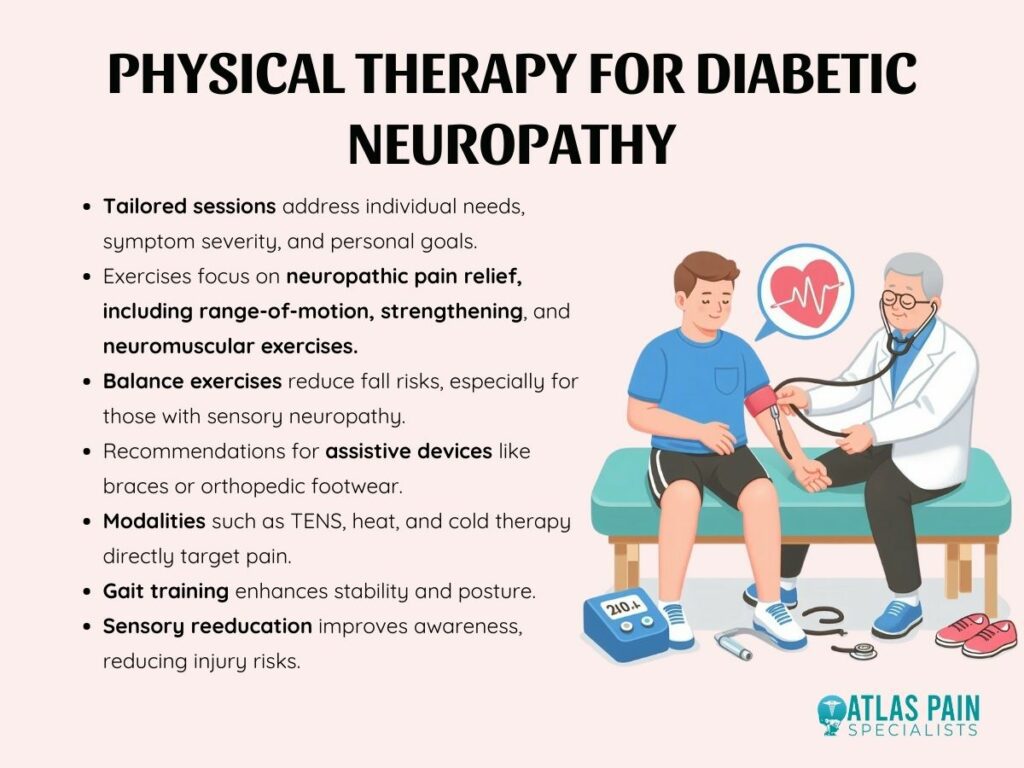
- Exercises for Nerve Pain Relief
Physical therapists design exercises to target neuropathic pain specifically. Range-of-motion exercises help improve flexibility and reduce stiffness while strengthening exercises enhance muscle support around affected nerves.
Neuromuscular exercises focus on improving nerve signaling and coordination, contributing to pain relief over time.
- Techniques for Improving Mobility
For individuals with diabetic neuropathy, maintaining mobility is crucial to preventing complications and promoting independence. Physical therapists may incorporate balance exercises to reduce the risk of falls, especially for those with sensory neuropathy affecting proprioception.
They may also recommend assistive devices such as braces or orthopedic footwear to enhance stability and reduce the risk of injuries.
- Modalities for Pain Management
Physical therapists may utilize various modalities to address neuropathic pain directly. Low-voltage electrical currents are applied to activate nerves by transcutaneous electrical nerve stimulation (TENS), which reduces pain.
Heat and cold therapy can also be employed to alleviate discomfort and reduce inflammation in targeted areas.
- Gait Training
Diabetic neuropathy can affect gait and coordination. Physical therapists assess walking patterns and may implement gait training to enhance stability and reduce the risk of falls.
This includes exercises and strategies to improve posture, stride length, and overall walking mechanics.
- Sensory Reeducation
Individuals with diabetic neuropathy may experience altered sensations, such as numbness or tingling. Sensory reeducation techniques aim to improve the brain's interpretation of sensory information, promoting better awareness of the body's position and movement.
This can be particularly beneficial in preventing injuries related to decreased sensation.
- Alternative Therapies
These approaches, rooted in various traditional and holistic practices, aim to address pain, improve well-being, and enhance overall quality of life. Integrating alternative therapies into a comprehensive pain management plan requires consideration of individual preferences, safety, and potential interactions with existing treatments.
Furthermore, different people may respond differently to these therapies, so what works for one person may not work for another.
- Acupuncture
In the ancient Chinese medical art of acupuncture, tiny needles are inserted into certain bodily locations. It is thought that by using this technique, the body's Qi (energy flow) can be more evenly distributed.
According to studies, acupuncture may reduce neuropathic pain by modulating nerve signals and stimulating the production of endorphins, the body's natural analgesics.
- Massage Therapy
By manipulating soft tissues, massage therapy helps people relax, release tension in their muscles, and increase circulation; for those who have diabetic neuropathy, particular massage techniques can be used to target the areas that are affected, thereby reducing pain and increasing overall comfort.
- Biofeedback
Biofeedback is a technique that helps individuals gain voluntary control over physiological processes, such as heart rate, muscle tension, and skin temperature. By providing real-time feedback, biofeedback allows individuals to learn how to influence these processes.
In the context of diabetic neuropathy, biofeedback may help individuals manage stress, reduce muscle tension, and potentially modulate their perception of pain.
- Herbal Remedies
Certain herbal remedies and supplements have been explored for their potential benefits in managing neuropathic pain. For example, alpha-lipoic acid, an antioxidant, has shown promise in reducing symptoms of diabetic neuropathy.
However, it's crucial to approach herbal remedies with caution, as their efficacy and safety can vary.
- Mind-Body Practices
Mind-body practices, including meditation, yoga, and tai chi, focus on the connection between the mind and body. These practices may help individuals with diabetic neuropathy manage stress, improve relaxation, and reduce the perception of pain.
Mindfulness-based stress reduction (MBSR) programs, for example, have demonstrated benefits in chronic pain management.
The Importance of a Multidisciplinary Approach
Diabetic neuropathy is a complex condition that extends beyond the realms of a single medical discipline. To effectively address the complex nature of neuropathic pain, provide all-encompassing care, and improve overall outcomes for patients with diabetes, a multidisciplinary strategy involving collaboration among diverse healthcare experts is necessary.
Collaborative Care Involving Healthcare Professionals
The management of diabetic neuropathy necessitates the expertise of a diverse group of healthcare professionals, each contributing unique insights and interventions. Endocrinologists play a central role in overseeing diabetes management, ensuring optimal blood sugar control, and preventing further nerve damage.
Neurologists bring specialized knowledge in understanding and addressing nerve-related issues, while pain management specialists offer expertise in tailoring interventions to alleviate neuropathic pain.
Collaboration extends to other allied health professionals, such as physical therapists, occupational therapists, and podiatrists.
- Physical therapists focus on enhancing mobility and implementing targeted exercises, while occupational therapists help individuals adapt to daily activities despite neuropathic challenges.
- Podiatrists specialize in foot care, which is crucial for preventing complications such as ulcers and infections.
Patient Education on Self-Management
Healthcare providers, including nurses, dietitians, and diabetes educators, play pivotal roles in educating individuals about self-management strategies. This includes guidance on medication adherence, blood sugar monitoring, and lifestyle modifications.
Empowering individuals with the knowledge and skills to participate in their care actively fosters a sense of control and self-efficacy. Moreover, educating individuals about the progressive nature of diabetic neuropathy, potential complications, and the importance of early intervention enhances awareness and encourages proactive health-seeking behaviors.
Psychological Support and Counseling
Living with chronic pain, such as that associated with diabetic neuropathy, often takes a toll on mental health. Integrating psychological support and counseling into the multidisciplinary approach is crucial for addressing the emotional and psychological aspects of neuropathic pain.
Psychologists, psychiatrists, or mental health counselors can assist individuals in coping with the challenges of chronic pain, managing stress, and addressing any comorbid mental health conditions. Furthermore, support groups and peer counseling can allow individuals to share experiences, exchange coping strategies, and foster a sense of community.
The Role of Support Systems in Pain Management
As we explore the many approaches, it becomes clear that diabetic neuropathy affects people's emotional and psychological health in addition to their physical health. The significance of a multidisciplinary approach is recognized, along with the cooperative efforts of medical professionals, the educational process that empowers individuals, and the critical function of psychological support. It takes a team to manage diabetic neuropathy; knowledge of the condition, patient experience, and emotional resilience all contribute to the task. We emphasize the need to have a strong support system to understand the complex nature of diabetic neuropathy fully.
About Dr. Sean Ormond