Understanding the Different Types of Abdominal Pain
Abdominal pain, a common complaint among many individuals, can range from a mild stomachache to severe acute pain. The abdomen houses various organs, including the stomach, liver, pancreas, intestines, and reproductive organs, and pain in this area can be a symptom of many different conditions.
In this article, we will explore the four different types of abdominal pain - visceral, parietal, referred, and colicky - delving into their unique characteristics, causes, and implications for treatment. Understanding these distinctions is crucial for effective diagnosis and pain management.
1. Visceral Pain
Visceral pain is a type of abdominal pain that arises from the internal organs, also known as the viscera. It's typically characterized by a deep, aching sensation that may be difficult to pinpoint exactly. This pain is usually not localized, meaning it's hard to identify the precise area of discomfort.
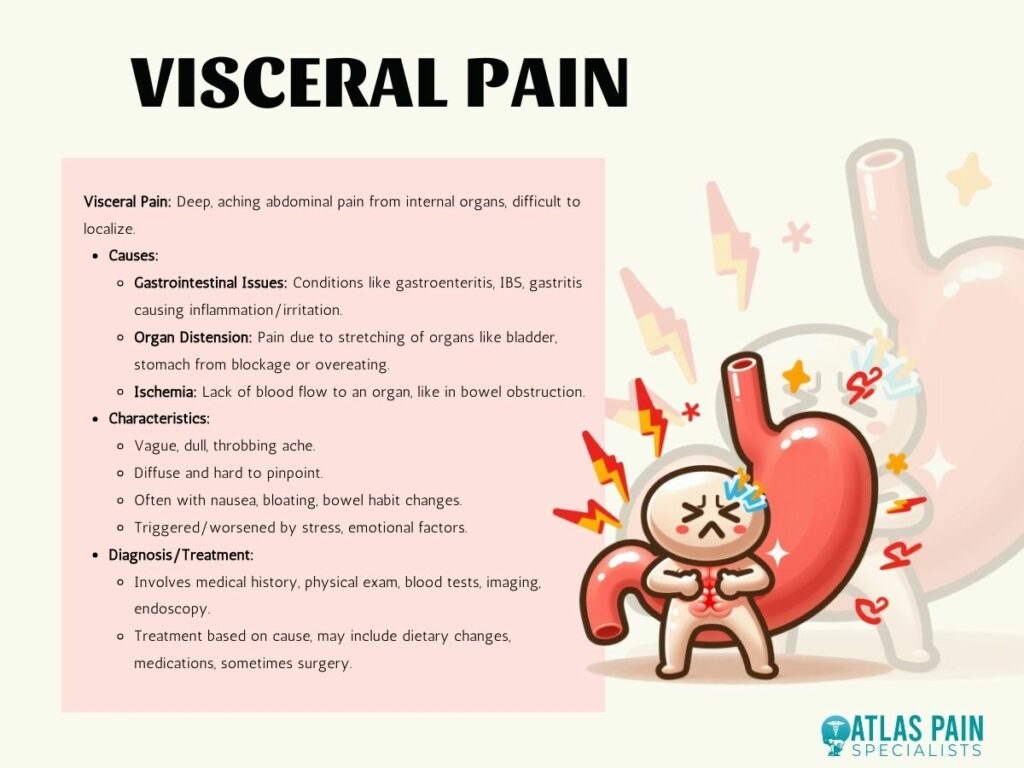
Causes of Visceral Pain
- Gastrointestinal Issues: Conditions like gastroenteritis, irritable bowel syndrome (IBS), and gastritis can lead to visceral pain. These conditions often cause inflammation or irritation in the stomach, intestines, or other digestive organs.
- Organ Distension: When an organ, such as the bladder or stomach, is stretched, visceral pain can occur. This might be due to a blockage, overeating, or other factors that cause an organ to expand beyond its normal size.
- Ischemia: A lack of blood flow to an organ, known as ischemia, can also cause visceral pain. This might happen in conditions like a bowel obstruction.
Characteristics of Visceral Pain
- It is often described as a vague, dull, or throbbing ache.
- The pain can be diffuse and hard to pinpoint.
- It may be associated with other symptoms like nausea, bloating, and changes in bowel habits.
- Visceral pain is often triggered or worsened by stress or emotional factors.
Diagnosis and Treatment
Diagnosing visceral pain typically involves a thorough medical history and physical examination. Blood tests, imaging (like ultrasound or CT scans), and endoscopy might be used to identify the underlying cause. Treatment depends on the specific diagnosis but may include dietary changes, medications to treat infections or reduce inflammation, and in some cases, surgery.
2. Parietal Pain
Parietal pain is a specific type of abdominal pain associated with the parietal peritoneum, which is the lining of the abdominal cavity. This pain is more localized and intense than visceral pain and is often aggravated by movement or touch.
Causes of Parietal Pain
- Inflammation of the Peritoneum: Conditions like peritonitis, where the peritoneal lining becomes inflamed, typically cause parietal pain. This can be due to infection, injury, or a perforated organ.
- Surgical Incisions: Postoperative patients may experience parietal pain around surgical incisions in the abdominal area.
- Trauma or Injury: Direct trauma to the abdominal wall can result in parietal pain. This might include injuries from accidents, sports, or physical activities.
- Infection or Abscess: Localized infections or abscesses in the abdominal cavity can also lead to parietal pain.
Characteristics of Parietal Pain
- Parietal pain is usually sharper and more easily pinpointed than visceral pain.
- It tends to worsen with movement, coughing, or sneezing, making it more intense.
- The pain is often described as a steady, aching sensation.
- It might be localized to a specific area in the abdomen, depending on the underlying cause.
Diagnosis and Treatment
The diagnosis of parietal pain typically involves a physical examination, particularly noting the pain's response to touch or movement. Diagnostic imaging like CT scans, MRIs, or ultrasounds can help identify the exact cause. Blood tests may also be used to check for signs of infection or inflammation.
Treatment for parietal pain depends on its cause. It may include antibiotics for infections, pain management strategies, and sometimes surgical intervention if there's a need to address an underlying issue like an abscess or perforation.
3. Referred Pain
Referred pain is a type of pain perceived at a location other than the site of the painful stimulus. It occurs when nerve fibers from regions of high and low sensation converge on the same nerve cells in the spinal cord, allowing pain from an internal organ to be mistakenly interpreted by the brain as coming from a completely different part of the body.
Causes of Referred Pain
- Gallbladder Issues: One of the most common examples of referred pain is gallbladder pain, often felt in the right shoulder or back.
- Heart Conditions: Angina or a heart attack may cause referred pain in the neck, jaw, or arms.
- Kidney Problems: Kidney stones or infections might cause pain that is felt in the lower abdomen or groin area.
- Lung and Diaphragm Issues: Conditions affecting the lungs or diaphragm can cause referred pain in the shoulder or upper abdominal area.
Characteristics of Referred Pain
- Referred pain is typically experienced away from the source of the problem.
- Depending on the underlying condition, it might feel dull and aching or sharp and intense.
- This type of pain can be misleading, as it does not align with the actual location of the problem.
Diagnosis and Treatment
The diagnostic process for referred pain involves a detailed medical history and a thorough physical examination. Doctors might consider various conditions based on the location of the pain and associated symptoms. Diagnostic imaging may be necessary, like ultrasounds, X-rays, or MRIs, and other tests like ECGs for heart evaluation.
Treatment for referred pain involves addressing the underlying cause. For instance, gallbladder issues may require dietary changes or surgery, while heart conditions might necessitate medication or more invasive treatments.
4. Colicky Pain
Colicky pain is a type of abdominal pain that comes in waves, characterized by its waxing and waning nature. It is often sudden in onset and can be extremely intense. Colicky pain is usually associated with the contraction of hollow organs, such as intestines or bile ducts, as they attempt to relieve an obstruction or irritation.
Causes of Colicky Pain
- Gastrointestinal Blockages: Conditions like intestinal obstruction or severe constipation can lead to colicky pain as the intestines attempt to move contents past the blockage.
- Kidney Stones: The movement of kidney stones through the urinary tract is a common cause of colicky pain, often felt in the back or side.
- Gallstones: Similar to kidney stones, gallstones can cause colicky pain as the body tries to pass them through the bile duct.
- Bowel Spasms: Irritable bowel syndrome (IBS) and other disorders that cause spasms in the intestines can also lead to colicky pain.
Characteristics of Colicky Pain
- The pain is typically spasmodic, meaning it comes and goes in waves.
- It can range from mild to severe in intensity.
- Colicky pain is often accompanied by other symptoms, such as nausea, vomiting, and sweating.
- The pain may cause restlessness, with patients often moving around to find a comfortable position.
Diagnosis and Treatment
Diagnosing colicky pain involves a detailed patient history and physical examination. Diagnostic tests such as ultrasounds, X-rays, and CT scans often identify the cause. For suspected kidney or gallstones, an MRI or a specialized ultrasound might be recommended.
Treatment focuses on relieving the underlying cause of the pain. For kidney or gallstones, this may include pain management, hydration, and medications to facilitate the passage of stones. In cases of intestinal blockages, more urgent medical or surgical intervention may be required.
In Summary
Understanding the different types of abdominal pain is crucial in identifying the underlying causes and determining the most effective treatment. Whether it's visceral, parietal, referred, or colicky pain, each type has its unique characteristics and implications.
At Atlas Pain Specialists, we prioritize accurate diagnosis and personalized treatment plans. We recognize that abdominal pain can significantly impact quality of life, and our dedicated team is committed to providing comprehensive care.
By addressing not just the symptoms but also the root causes of abdominal pain, we strive to enhance our patients' overall well-being and health. Remember, if you're experiencing persistent or severe abdominal pain, seeking medical attention is essential for proper care and relief.
About Dr. Sean Ormond